Challenges of Migraine Diagnosis
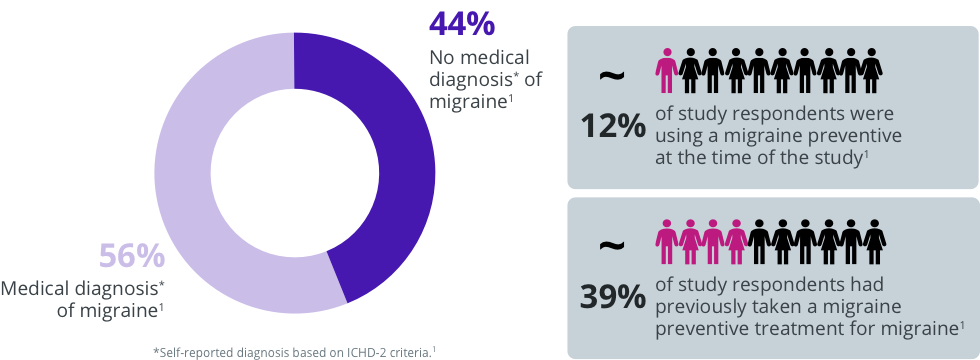
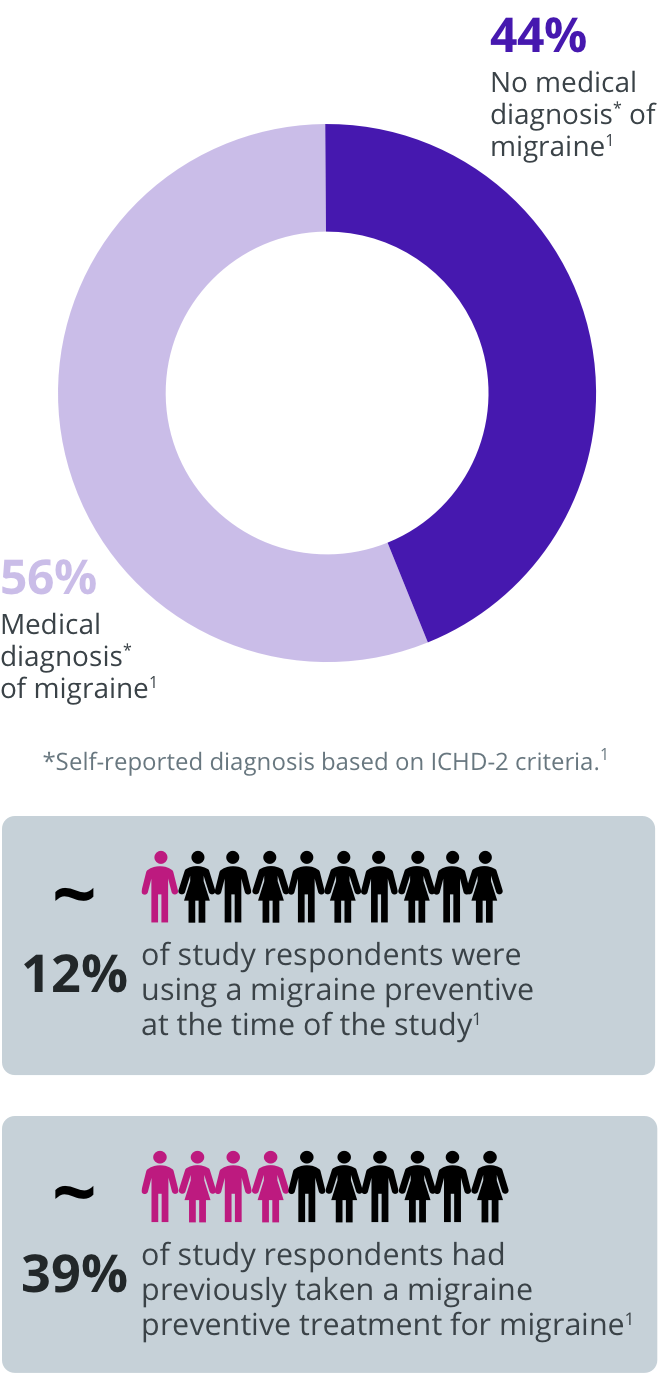
Although migraine is a common disease with substantial impact, it is underdiagnosed and undertreated.1-3
In the American Migraine Prevalence and Prevention Study (N = 18,968), a substantial proportion of people who met the International Classification of Headache Disorders, second edition (ICHD-2) criteria for migraine reported never having received a medical diagnosis of migraine.1
![]()
Furthermore, in an observational study (N = 2,991), 88% of people with a self-diagnosis or medical diagnosis of sinus headache were classified with migraine-type headache per International Headache Society (IHS) criteria.2
TEST YOUR KNOWLEDGE
Approximately what percentage of people in the United States
meeting criteria for
migraine have not received a diagnosis?
A
B
C
D


Correct answer:
A
ICHD-3 Diagnostic Criteria for Migraine
Migraine diagnosis is described in the third edition of the ICHD (ICHD-3), developed by the IHS.4
To be diagnosed with migraine, a patient should have experienced at least 5 attacks that fulfill the following criteria:4
Headache attack duration
Headache attack lasts 4–72 hours (when untreated or unsuccessfully treated)
Headache characteristics
Headache has ≥ 2 of the following 4 characteristics:
- Unilateral location
- Pulsating quality
- Moderate or severe pain intensity
- Aggravation by or causing avoidance of routine physical activity (eg, walking or climbing stairs)
Non-headache symptoms
During headache, the patient has ≥ 1 of the following:
- Nausea and/or vomiting
- Photophobia and phonophobia
Not better accounted for by another ICHD-3 diagnosis
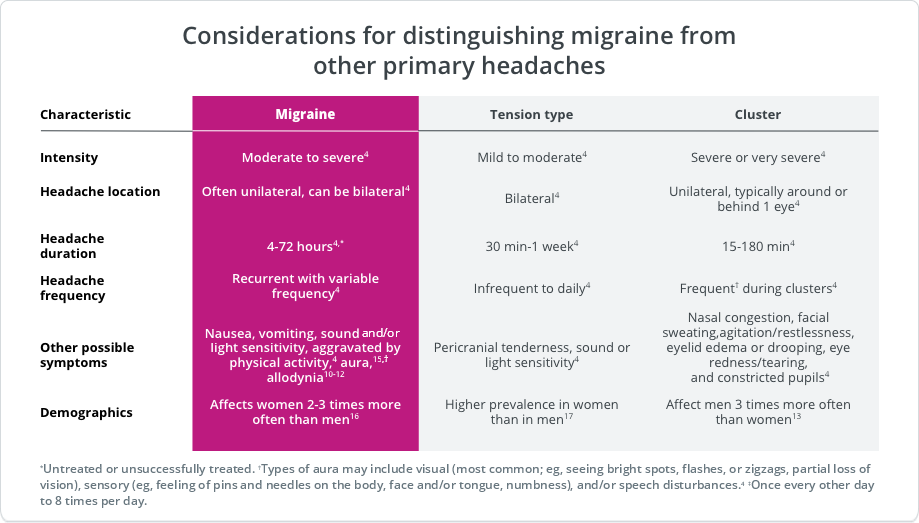
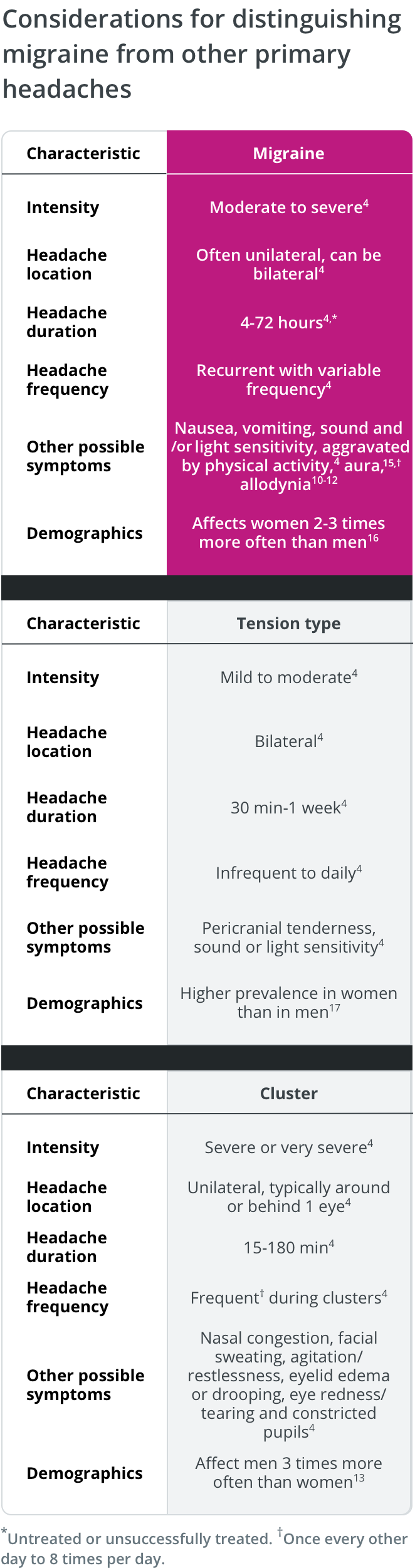
Considerations for the Differential Diagnosis of Migraine
An accurate diagnosis of migraine depends on obtaining an accurate patient history.5 However, because of overlapping symptoms, differentiating migraine from other headache disorders can be challenging.2,6-9
Characteristic symptoms of migraine facilitate differential diagnosis from other primary headache disorders, including tension-type and cluster headache.4
Key distinctive features of migraine are:4,10-12
- Unilateral location
- Long duration (4‐72 hours)
- Frequency
- Associated symptoms such as nausea and/or vomiting
- Sensitivity to light and sound or to touch
While these are distinctive features, migraine can also be bilateral and may not be associated with nausea.13,14
TEST YOUR KNOWLEDGE
Sheila* experiences frequent headaches of moderate pain intensity (usually 5 to 6 on a scale of 10). Each headache can last as long as 2 days, and during these attacks, she often feels nauseated and reports being sensitive to both light and sound, and that her head is sensitive when touched. These symptoms sometimes prevent her from maintaining her regular level of physical activity because she finds that being active, even if she’s not exerting herself, aggravates the symptoms. She was previously and incorrectly diagnosed with tension-type headache—the correct diagnosis is migraine. Which key feature(s) exclude tension-type headache as Sheila’s* diagnosis? Select all that apply.
A
B
C
D
E
F


Correct answer:
A, B, C
*This is a hypothetical patient case.
Available Tools for Migraine Diagnosis
Both general headache and migraine-specific tools are available, which may be used concurrently to help exclude secondary headache and diagnose primary headache, including migraine.5,9
Examples of tools that may facilitate migraine diagnosis in clinical practice
GENERAL
MIGRAINE-SPECIFIC
Example of tools that may facilitate migraine diagnosis in clinical practice
GENERAL
Headache diary6
Often tracks:
- Headache frequency
- Intensity
- Duration
- Associated features
SNOOP5,9,*
- Systemic symptoms/signs/ disease
- Neurologic symptoms or signs
- Onset sudden
- Onset (> 50 years)
- Pattern change
Excludes secondary headaches
Brief Headache Screen (BHS)5
Distinguishes:
- Episodic headaches
- Daily headaches
- Medication overuse headache (MOH)
ID-MigraineTM 5,18
3 simple questions on:
- Limited activities
- Sickness to stomach (ie, nausea)
- Light sensitivity
MIGRAINE-SPECIFIC
Headache diary4
Often tracks:
- Headache frequency
- Intensity
- Duration
- Associated features
SNOOP5,9,*
- Systemic symptoms/signs/ disease
- Neurologic symptoms or signs
- Onset sudden
- Onset (> 50 years)
- Pattern change
Excludes secondary headaches
Brief Headache Screen (BHS)5
Distinguishes:
- Episodic headaches
- Daily headaches
- Medication overuse headache (MOH)
ID-MigraineTM 5,18
3 simple questions on:
- Limited activities
- Sickness to stomach (ie, nausea)
- Light sensitivity
Trademarks and registered trademarks are the property of their respective owners.
*SNOOP is a diagnostic screener for secondary headache, including systemic and neurologic symptoms, onset, other associated conditions, and prior headache history.
Migraine Classification
Diagnoses of migraine can be refined based on the frequency of monthly migraine days (MMDs) and monthly headache days (MHDs). Patients with < 15 MMDs or MHDs have episodic migraine, and those with ≥ 15 MHDs, of which ≥ 8 are MMDs, have chronic migraine.4,19
Because of the cyclical nature of migraine, headache day frequency for individual patients may change over time.20 Clinical findings suggest that migraine can progress over time.21,22 Approximately 3% of patients with migraine transition from episodic migraine (< 15 headache days per month) to chronic migraine (≥ 15 headache days per month for over 3 months, with features of migraine ≥ 8 days per month) every year. 4,19,21 Conversely, one study showed that over a 2 year period, 26% of patients with chronic migraine transitioned back to episodic migraine.23 Several factors have been associated with this progression, including the presence of cutaneous allodynia, the presence of nausea, and the effectiveness of acute medication, with less optimal responses increasing the likelihood of a patient's disease progressing over time.24,25
Transitioning between episodic migraine and chronic migraine may have implications for migraine classification and diagnosis.20
Medication Overuse Headache
Several drug classes are available or in development for the acute or preventive treatment of migraine.19,26-28 Treatment decisions may be impacted by a drug’s safety and efficacy profile, patients’ comorbidities and concomitant medications, and patient preference.19,29,30
Both migraine-specific acute medications (eg, triptans, ergotamines, and ditans)19,31 and non–migraine-specific acute medications (eg, analgesics and nonsteroidal anti-inflammatory drugs)30 are approved by regulatory agencies and/or recommended by professional society guidelines for relief from migraine attacks. According to the American Headache Society, opioids and barbiturates are not recommended for regular use because of their addiction and abuse potential.19,26,32
Although some acute medications are indicated and/or recommended for aborting attacks, acute treatments can be overused, potentially leading to medication overuse headache (MOH), a type of secondary headache disorder.4 MOH may occur with acute migraine medications, but is common with narcotics and barbiturates; this is another reason why AHS guidelines recommend that opioids and barbiturates generally be avoided for migraine treatment.19,26,32
Approximately 50% of patients with chronic migraine have MOH that may revert to episodic headache after drug withdrawal.4 As such, it is recommended that acute treatments be limited to an average of 2 headache days19 per week, and preventive treatment is considered for patients observed exceeding this limit.30 Also, it is advised that acute treatments should not be used in anticipation of a migraine attack.33
ICHD-3 Criteria for MOH4,19

Headache occurring on ≥ 15 days per month in a patient with a preexisting headache disorder

Regular overuse for > 3 months of ≥ 1 drug that can be taken for acute and/or symptomatic treatment of headache, with medication overuse defined as:

≥ 10 days per month for ergot derivatives, triptans, opioids, combination analgesics,* and a combination of drugs from different classes that are not individually overused

≥ 15 days/month for nonopioid analgesics, acetaminophen, and NSAIDs

Not better accounted for by another diagnosis
*Drugs of ≥ 2 classes, each with an analgesic effect or acting as adjuvants.
TEST YOUR KNOWLEDGE
The AHS considers that acute treatment can be effective in
reducing pain,
symptoms, and disability associated with migraine attacks;
however, the 2021 AHS
guidance cautions that overuse of acute medications should be
avoided.1
According to the ICHD-3, what are the criteria for acute
medication overuse for a
person with a primary headache disorder? Select all that apply.
A
B
C
D
E


Correct answer:
A, B
AHS, American Headache Society; ICHD-3, International Classification of Headache Disorders, 3rd edition; NSAID, nonsteroidal anti-inflammatory drugs.
1. American Headache Society. Headache. 2021;61:1021-1039.
