Expert Video: Potential Impact of Migraine on Brain Structure and Function
What are the potential implications of migraine on brain structure and function?
Expert Christoph Schankin, MD, discusses the potential implications of migraine on brain structure and function in this short video

Potential Impact of Migraine on Brain Structure and Function
Migraine Neuroimaging Techniques
Clinical studies have used neuroimaging techniques to assess the structural and functional effects of migraine.1-3

Structural Imaging
-
Used to visualize anatomic properties of the brain, including:1
- Size and volume of brain structures1
- Thickness of cortical areas (eg, gray matter)1,4
- White matter tracts4,5
- Used to detect brain damage and abnormalities1
- Includes magnetic resonance imaging (MRI), computed tomography (CT), and diffusion tensor imaging (DTI)1

Functional Imaging
- Used to define regions that are active during specific behaviors and cognitive activities1,6
- Can include the study of stimuli-induced responses or “at rest”6,7
-
Indirect measure of neural activity in the brain:
- Functional magnetic resonance imaging (fMRI)–blood oxygen level–dependent (BOLD) signal1,6
- Positron emission tomography (PET) – metabolism associated with performing a task/behavior1,6
Imaging studies suggest that migraine is associated with changes in brain structure and function.2,3,8
TEST YOUR KNOWLEDGE
Which changes to brain structures have been observed in patients with migraine? Select all that apply.
A
B
C


Correct answer:
A, B

Structural Imaging Studies
Structural changes in brain regions involved in pain processing have been reported in patients with migraine.2,8
STUDY: Magnetic resonance imaging was used to investigate the differences in cortical mean thickness between patients with migraine without aura (n = 48) and healthy controls (n = 48).2
Patients with migraine display reduced density in cortical areas involved in pain processing.2,8
Compared with normal controls, patients with migraine exhibited decreased cortical thickness in the:2
- Bilateral cuneus
- Posterior cingulate
- Inferior parietal lobule
- Inferior frontal gyrus
- Middle temporal gyrus
Differences in cortical mean thickness between patients with migraine and healthy controls


![]()
Warm coloration indicates the brain regions showing an increased cortical mean thickness, and cold coloration indicates the brain regions showing a reduced cortical mean thickness in patients who have migraine without aura. The mapping threshold was set at P<0.05.
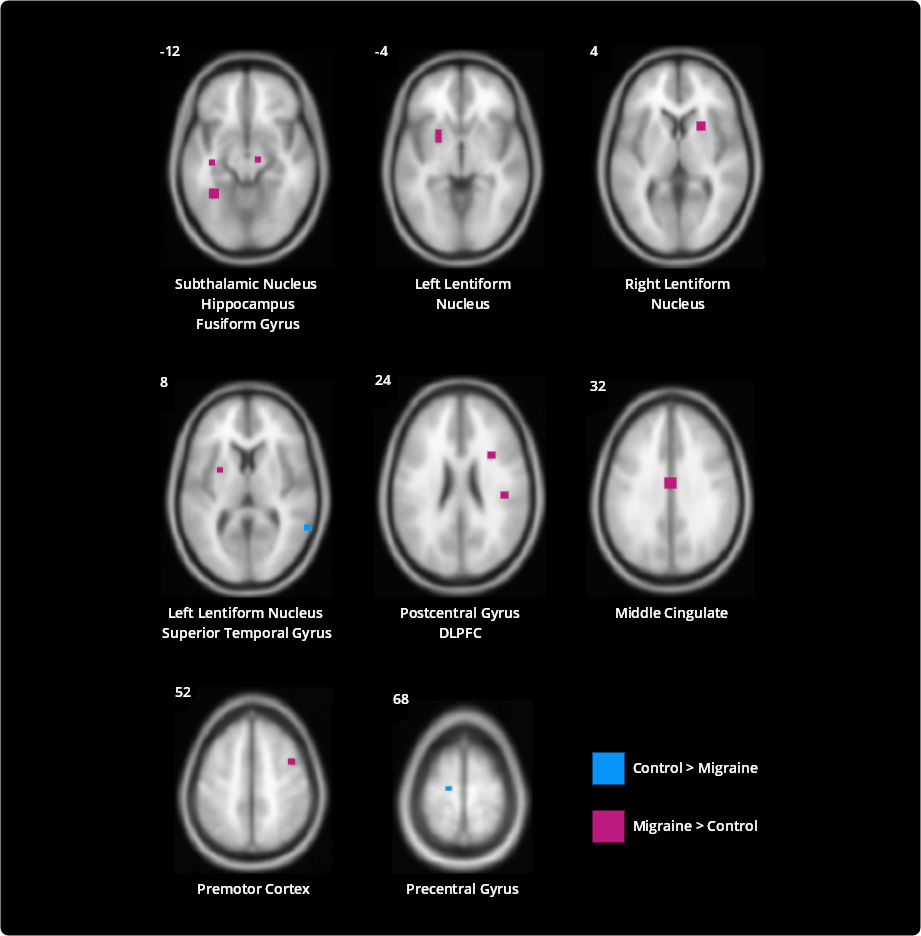
An analysis of patients with medication overuse headache (MOH) has shown that these patients display structural changes, such as gray matter texture abnormalities.9
STUDY: Structural MRI and 3-D texture analysis were used to compare features of the brains of patients with MOH (based on the International Classification of Headache Disorders, third edition beta [ICHD-3β] criteria, n = 44) with those of normal controls (n = 32).9
Compared with controls, the brains of patients with MOH showed altered textural features in the:9
- Cerebellar vermis
- Left cerebellum
- Left dorsolateral periaqueductal gray (L-dlPAG)
- Right parahippocampal gyrus (R-PHG)
- Left middle frontal gyrus (L-MFG)
- Right superior parietal lobule (R-SPL)
Scatter plot of texture parameters with clinical variables in MOH
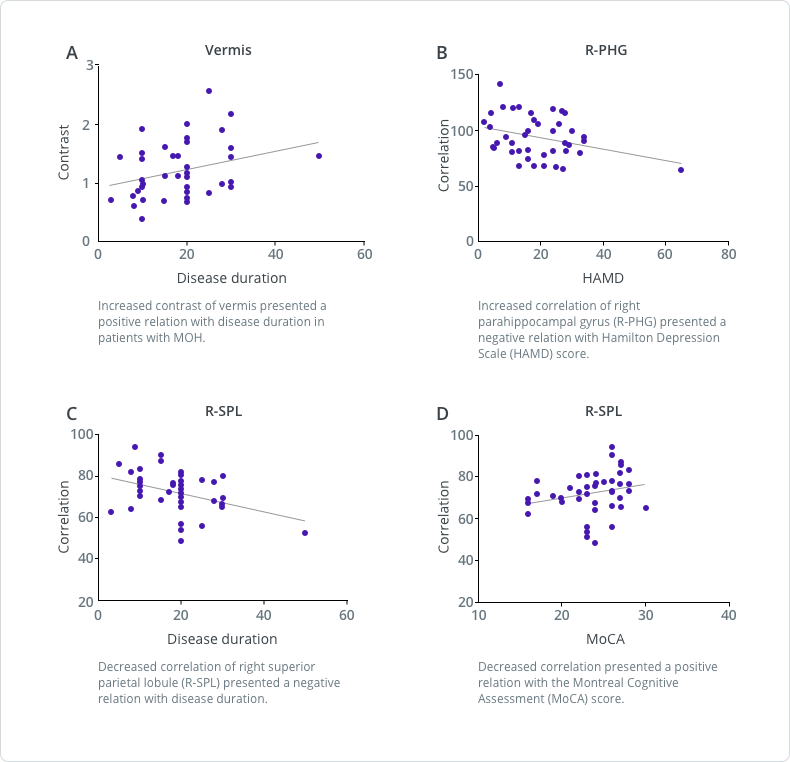
![]()

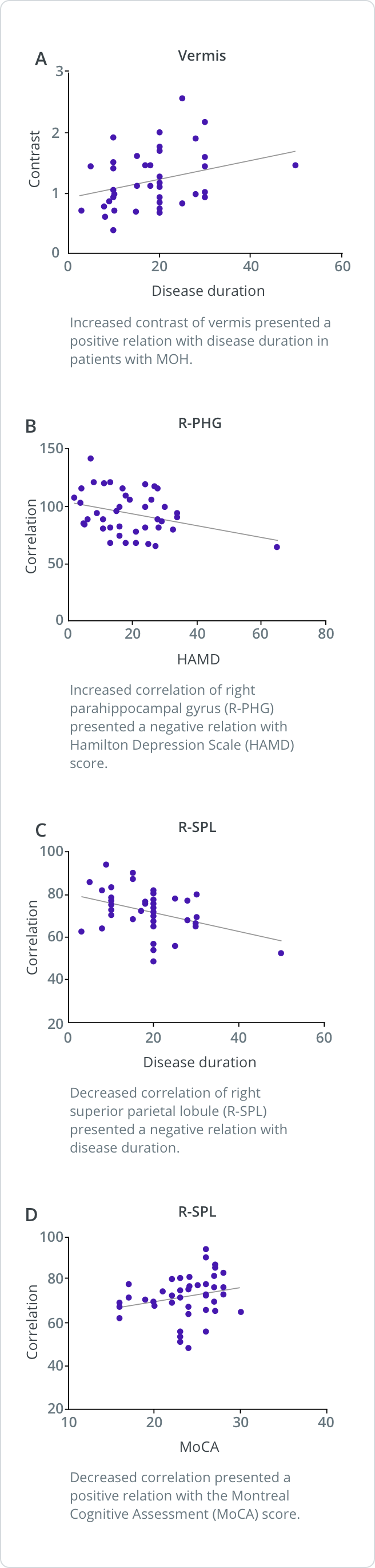
Functional Imaging Studies
Patients with migraine may also demonstrate functional changes, such as altered brain activation in the presence of pain stimulation.3
STUDY: Functional MRI was used to assess whole-brain responses to painful heat in 24 adult patients and 27 healthy controls.3
Several brain regions were differentially activated in patients with migraine.3
-
Areas with increased pain-induced activation:
- Lentiform nucleus
- Fusiform gyrus
- Subthalamic nucleus
- Hippocampus
- Middle cingulate cortex
- Premotor cortex
- Somatosensory cortex
- Dorsolateral prefrontal cortex
-
Areas with reduced pain-induced activation:
- Precentral gyrus
- Superior temporal gyrus
Noxious heat-induced activations differing between patients with migraine and control subjects
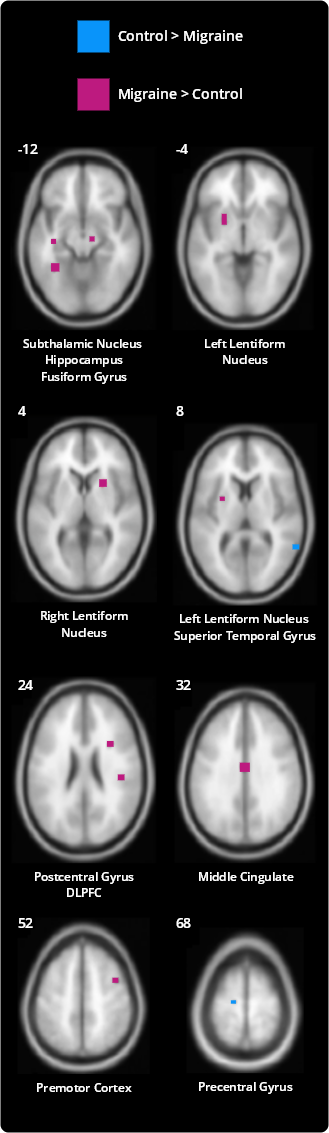
![]()
Several regions differentially activated in patients with migraine compared with control subjects (P<0.005, cluster corrected). Voxels colored red were more strongly activated in patients with migraine compared with control subjects. Voxels colored blue were more strongly activated in control subjects compared with patients with migraine. Numbers next to each axial slice represent the Z-coordinate. Slices are shown with the right side of the brain on the right.
The majority of regions with enhanced pain-induced activation in patients with migraine participate in cognitive aspects of pain perception. Enhanced cognitive pain processing in patients with migraine might reflect cerebral hypersensitivity related to high expectations and hypervigilance for pain.3
In the same functional imaging study just described, fMRI results showed an association between increased pain-induced activation and increased headache day frequency.3
Specifically, positive correlations between activation strength and headache frequency were observed in the:3
- Middle cingulate
- Right dorsolateral prefrontal cortex
- Left fusiform gyrus
- Left precentral gyrus
- Left hippocampus
Correlations between pain-induced activation and headache frequency
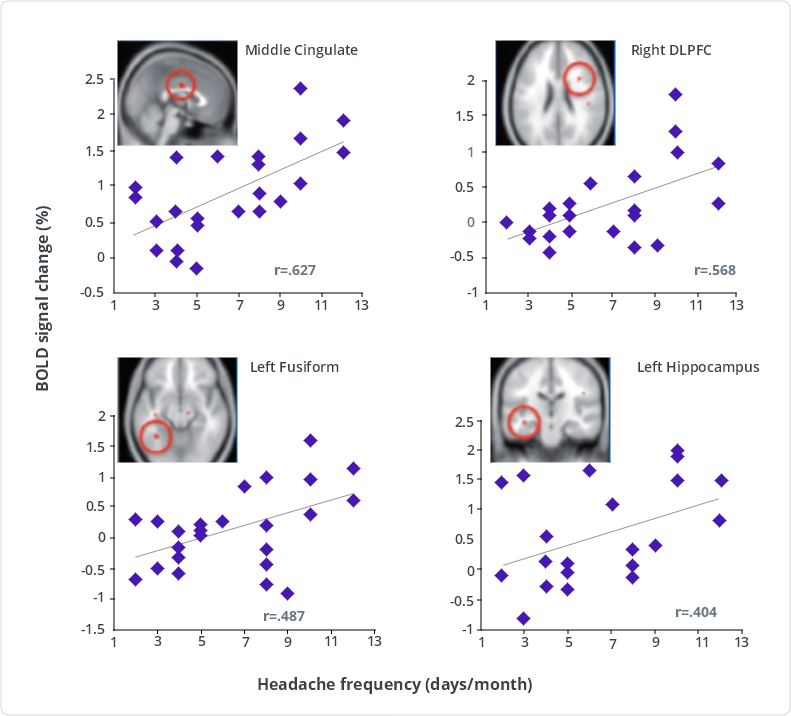
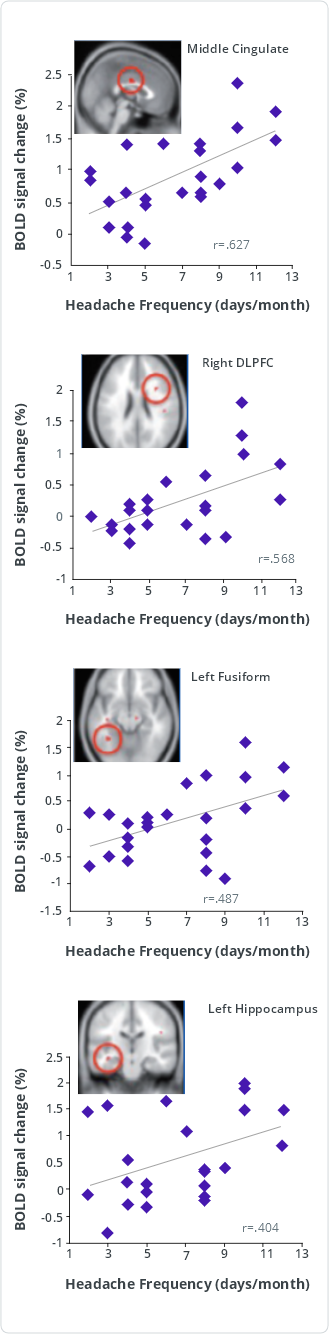
DLPFC = dorsolateral prefrontal cortex
Pain-induced activation of the middle cingulate, right dorsolateral prefrontal cortex, left fusiform gyrus, and left hippocampus significantly correlated (P<0.05, uncorrected) with headache frequency (days per month with headache). Following Benjamini-Hochberg correction for multiple comparisons allowing for a false-discovery rate of 5%, correlations with the middle cingulate and right dorsolateral prefrontal cortex were still significant.
These results suggest that atypical activation correlates with migraine burden.3
TEST YOUR KNOWLEDGE
What changes in brain structures are associated with increased headache day frequency or longer disease duration? Select all that apply.
A
B
C


Correct answer:
A, B, C
