AHS Treatment Recommendations
The American Headache Society (AHS) provides evidence-based recommendations for the
initiation of acute and preventive treatments.3
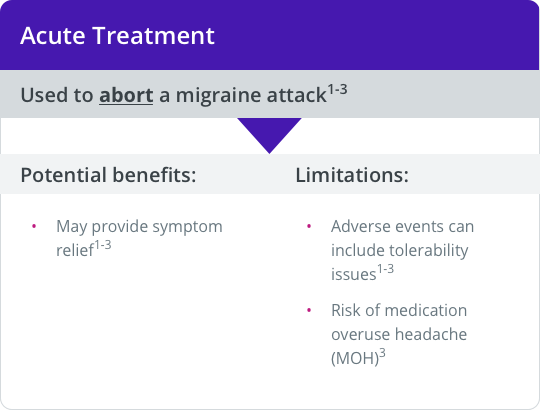
AHS Recommendations for Acute Treatment
According to AHS guidelines, all patients with a confirmed diagnosis of migraine should be offered a trial of acute pharmacologic and/or nonpharmacologic treatment.3
Goals of acute treatment include achieving rapid freedom from pain and associated symptoms and restored ability to function.3
Considerations for acute treatment include those related to efficacy, safety, tolerability, comorbidities, and concomitant medications.1,3
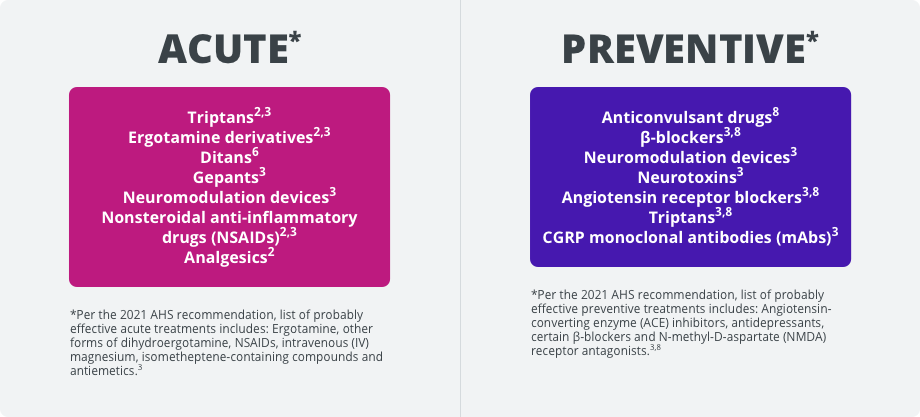
Migraine-specific and general pain medications are recommended for the acute treatment of migraine.1-3 Specifically, the AHS recommends the use of NSAIDs, nonopioid analgesics, or combination therapy for mild-to-moderate attacks and migraine-specific agents for moderate or severe attacks and mild-to-moderate attacks that respond poorly to nonspecific therapy.3
AHS-listed drugs for acute treatment of migraine with established efficacy3
General pain medications
- NSAIDs
- Combination analgesics
Acute migraine-specific medications
- Triptans
- Ergotamine derivatives
Recently approved acute treatments
Regardless of which acute treatment is prescribed, patients should be instructed to treat at the first sign of pain to improve the probability of achieving freedom from pain and reduce attack-related disability.3
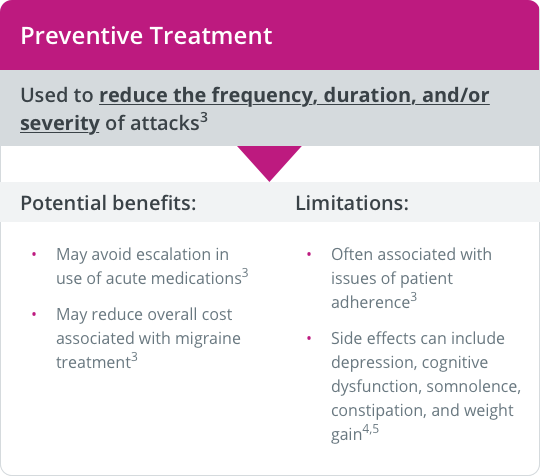
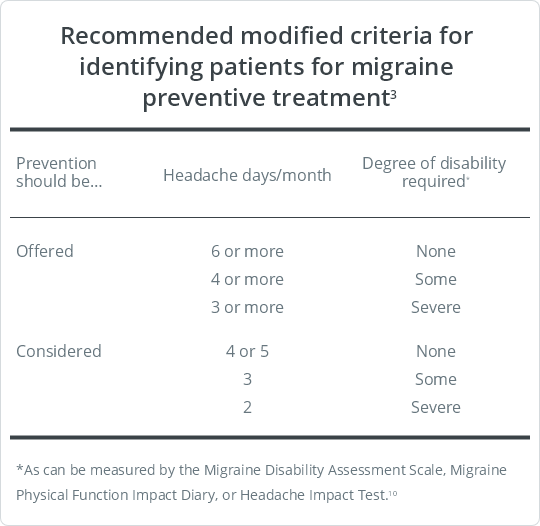
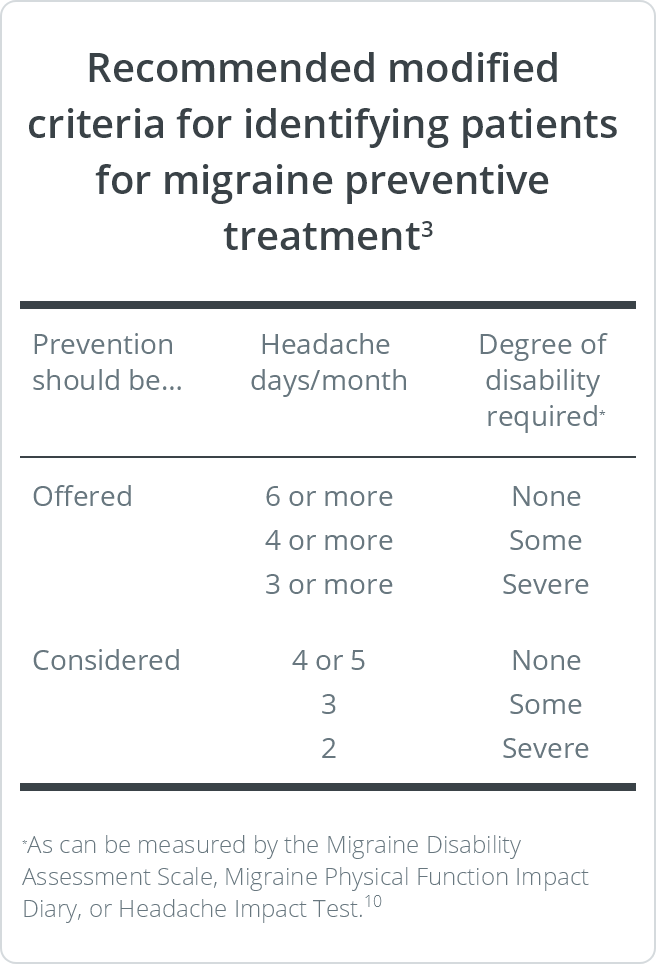
AHS Recommendations for Preventive Treatment
Preventive treatments—pharmacologic, interventional, biobehavioral, neurostimulation, nutraceuticals, and lifestyle modification—are important parts of the overall approach for a proportion of people with migraine, and multiple evidence-based guidelines are available.3 However, epidemiology data support that preventive treatment is underutilized, as only about one-third of patients with migraine who qualify for preventive treatment receive it.9,10
Preventive treatment is recommended for patients with elevated headache frequency, increased symptom severity, and/or impaired functioning.3